– ABRIDGED VERSION –
Published study April 10, 2021 at RESTCON Conference. Study partners where Weber State
University, McKayDee Hospital & i-Float Sensations, South Ogden, UT
Restricted Environmental Stimulation Therapy for Concussion Treatment
(RESTCON): a pilot study
S Moore DO 1 , H Emerson MD 2,3 , C Madsen MD MS 2,4
2 Department of Family Medicine, McKay-Dee Family Medicine Residency Program, Ogden, UT
3 Family Medicine, Tanner Clinic, Roy, UT
4 Team Physician, Weber State University, Ogden, UT
Funding: New faculty grant from the Weber State University Research Scholarship and Professional
Growth (RSPG) fund.
Keywords: REST, Sensory Deprivation, Concussion, mTBI, Post-concussion Syndrome
Biographical Note:
Scott Moore; academic clinical pathologist and professor of medical laboratory sciences Clark Madsen;
academic sports medicine physician and family medicine residency faculty Haleigh Emerson; community
family medicine physician.
ABSTRACT:
Objective: Evaluate Restricted Environmental Stimulation Therapy (REST) use in acute or chronic concussion.
Design: Prospective cohort study with two cohorts; acute (<6 weeks) and chronic (≤6 weeks) concussions. Subjects underwent 3 sessions of REST within 10 days monitoring symptoms before and after therapy.
Setting: University and community sports medicine clinics.
Participants: 8 patients with acute (N=5) and chronic (N=3) concussions between 18-59 years of age were recruited.
Main outcomes measured: Symptom scores (SCAT-5) before and after REST sessions and a post-study survey.
Results: Symptom scores decreased by an average of 18.8 points (±6.9, p =0.01) from pre- to post-float and dropped an average of 9 points ( p =0.02) between sessions. Patients were universally positive about their REST experience. Nausea was the most common adverse event (N=2) and all subjects responded that they recommended REST for concussion treatment after completing the study.
Conclusions: REST has the potential for symptomatic relief for patients with acute or chronic concussions. Further testing is required to determine the magnitude of effect, duration of symptom relief, and optimal frequency of REST.
INTRODUCTION:
Concussion treatment has evolved greatly over the past decade 1,2 . Further understanding of how injury occurs and how the brain recovers has led to numerous treatment modalities and protocols. Despite this, the mainstay of concussion treatment involves varying levels of rest, both cognitive and physical. Few studies have shown definitive recovery benefits from active interventions such as medication, activity, or therapy 3,4 . It is clear that excessive activity early on can worsen a patient’s concussion symptoms in the short term 5 . This has created an environment where active forms of rest could have an impact on patient recovery.
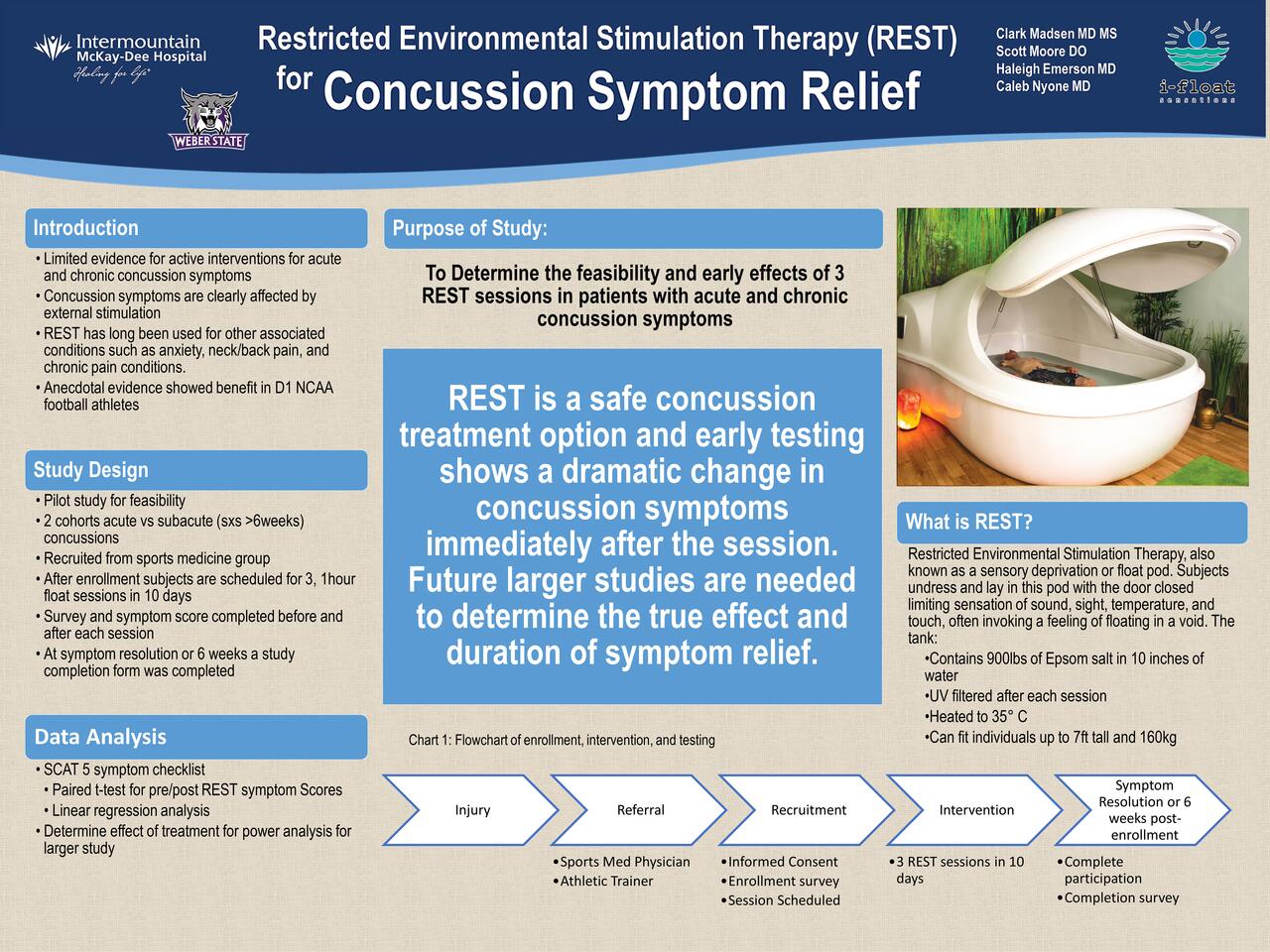
Restricted Environmental Stimulation Therapy (REST) has been a treatment used for decades with studied effects on addiction, anxiety, muscular pain, and pain tolerance but not on traumatic head injuries. Despite this, anecdotal reports from local football players who use REST were overwhelmingly positive. REST, also known as sensory deprivation tanks or “float tanks”, involves subjects laying in a specialized pod with a shallow pool of warm water containing high concentrations of Epsom salt (magnesium sulfate), Figure 1. The subject floats on top of the water and the sensations of temperature, sound, vision, and touch are all dampened. With minimal stimulation, subjects will often fall into a state of deep relaxation. We hypothesize that reducing stimulation and allowing for deep relaxation can have a positive effect on concussion symptoms.
METHODS:
The study protocol was approved by the IRB of Intermountain Healthcare and Weber State University. Subjects were 18 years or older and had a SCAT-5 graded symptom score of at least 20. … Subjects were recruited from a Sports Medicine clinic after clinical diagnosis of acute concussion (cohort 1) or chronic concussion, with symptoms lasting greater than 6 weeks (cohort 2). At enrollment, the subjects followed the pathway outlined in Figure 2 and were scheduled for 3 sessions of REST within a 10-day period. They also completed a symptom checklist (SCAT-5) before and after each REST session. After 6 weeks or resolution of their concussion symptoms, the subjects completed a final questionnaire regarding their experience with REST….
RESULTS:
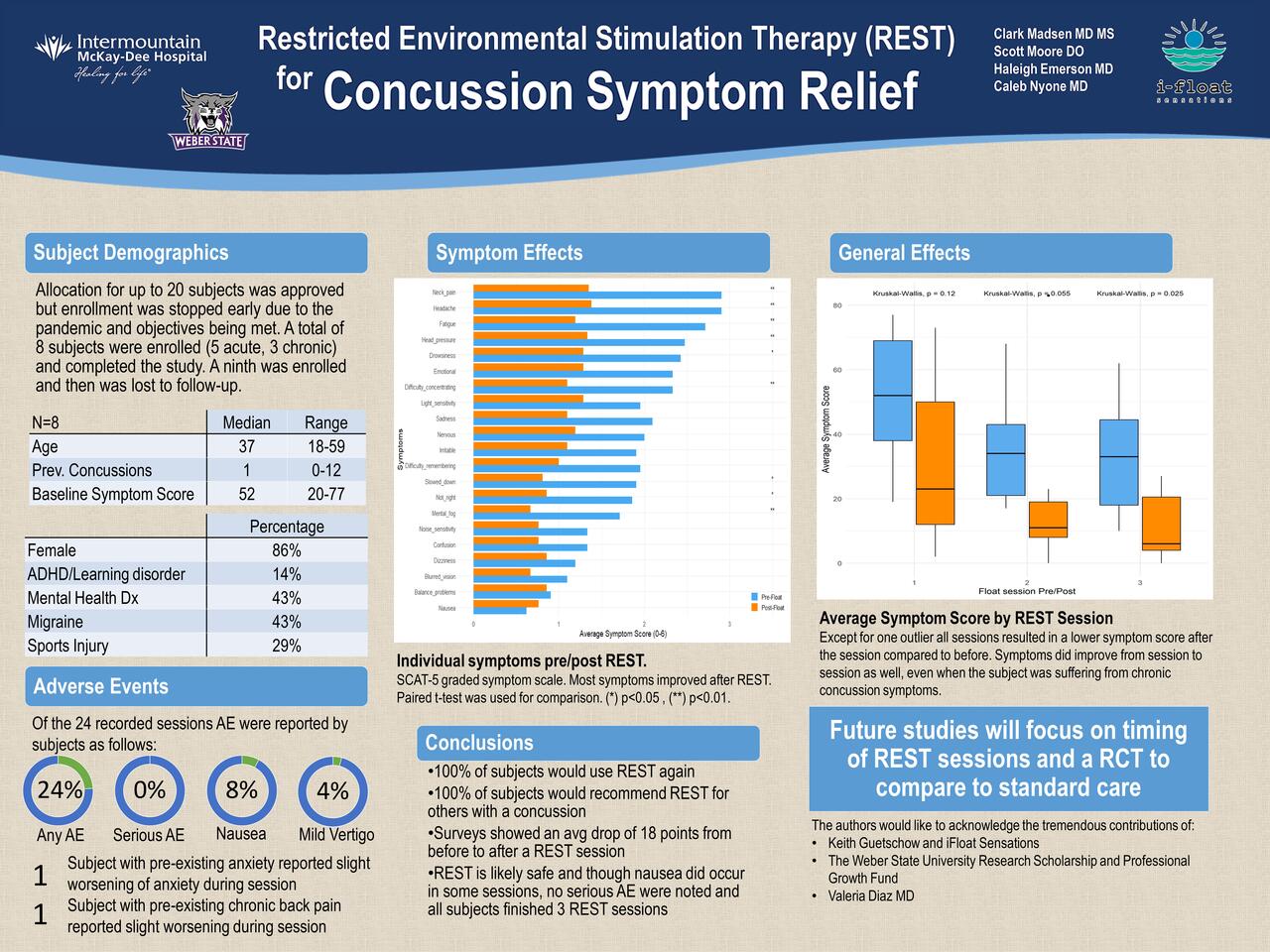
Eight subjects were enrolled; five with acute and three with chronic symptoms. … There was an average 18 point drop in symptom score from the pre- to post-REST assessment on the paired t-test (p<0.001). There was no significant difference seen in outcomes between the two cohorts, though this is likely limited based on sample size.
In linear regression analysis, there was also an 18 point average drop in the symptom score from before to after the float (p=0.008). This was concluded after controlling for days since injury, hours of sleep the previous night, and number of sessions performed. The number of sessions was also a significant predictor with the average symptom score dropping 9 points per session (p=0.02), …
A post-study survey of attitudes toward REST showed that all participants felt that they would recommend REST to a friend with a concussion. Most REST sessions had no adverse effects to report (76%). Two subjects had some nausea on their first session but not on others. … Interestingly one subject with acute concussion stated that REST also helped her neck and back pain, while one subject with chronic concussion noted that her neck and back pain were mildly worse during REST.
DISCUSSION:
All patients said that they would use floatation therapy again, would recommend it to a friend, and objectively felt better, with a lower post-REST symptom score compared to pre-REST. The effect increased progressively as the subjects completed more floats. …
An average of 18 point improvement in the SCAT-5 symptom score is clinically significant in the eyes of the authors and is recognized by the subjects who answered that they felt better after 86% of REST sessions.
Patients with chronic concussions had higher average symptom scores, more preexisting comorbidities, and were found to sleep fewer hours, which was expected based on prior work 6,7 . This study was unable to show a difference in effect for those with chronic or acute concussion symptoms but the mean symptom score dropped by 25 and 14 points in acute and chronic concussions respectively. The effect size of REST may be understated in this study as many subjects were reaching zero or near zero symptoms by the time they finished the REST session …
CONCLUSION:
REST in concussion appears to provide at least temporary relief from concussion symptoms. In this small cohort study a clear pattern of benefit has emerged. Further study is encouraged as REST does have the potential to become a standard treatment for concussion.
FIGURE 3 : Average symptom score by REST session
Except for one outlier all sessions resulted in a lower symptom score than initial presentation.
Symptom scores did improve from session to session as well.
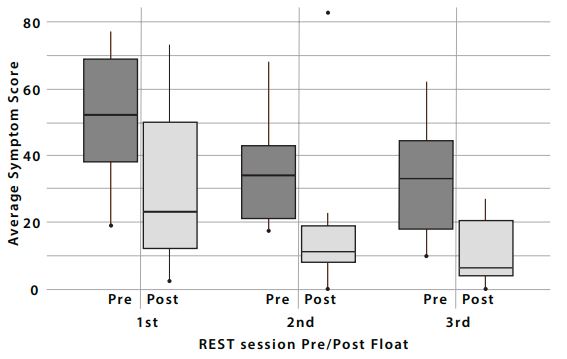
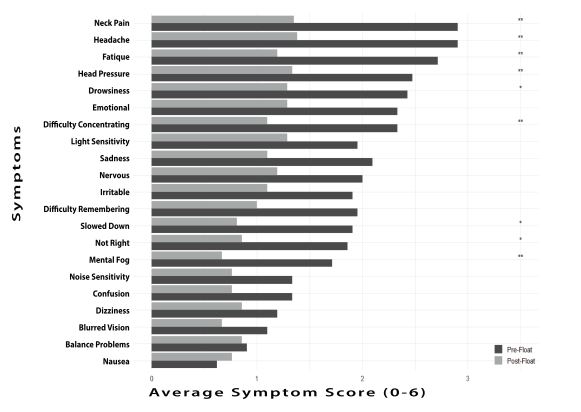
FIGURE 4: Individual symptoms pre/post REST.
SCAT-5 graded symptom scale. Most symptoms improved after REST. T-test was used for comparison.
(*) p<0.05 , (**) p<0.01.
i-Float Sensations LLC, 1490 e 5600 s, Suite 2, South Ogden, UT 84403 Ph: 801.888.6777
www.ifloatOgden.com
i-Float Sensations does an initial consultation prior to the first REST session and again after.
Call in if you wish to book a brief consultation session at no extra charge.
Total 4 initial floats in a two-week period is optimal.
Week 1 – (3) 1-hour float sessions
Week 2 – if symptoms come back (1) 1-hour float session
Week 3 and beyond Float as needed or at least once a month
After the initial 3 sessions another consultation is done.
An additional consultation may be done as week 2 protocol comes to an end.
We recommend at least one float a month or more as needed after week 3.
Notes:
For any kind of TBI and/or Concussion it is important to float as soon as possible after the initial injury and follow all doctor prescribed protocols. Symptoms will deplete substantially after each float session but will come back to a lesser degree the next morning. It is important to do the 3 float sessions as outlined above with the 4th float as an option if some symptoms still linger.
Don’t eat for at least 2 hours prior to floating.
Take any medication at least 4 hours prior to floating.
Better to come in slightly dehydrated or least don’t drink a lot of liquid prior.
Do not float if you have any severe cuts or open wounds.